- HYGEIA
- Vision & Mission
- Timeline
- Organizational structure
- Press Releases
- Social responsibility
- Awards and Distinctions
- Human Resources
- Scientific & Training activities
- Articles – Publications
- Our Facilities
- Magazines
- Healthcare Programs
- Doctors
- Services
- Medical Divisions & Services
- Imaging Divisions
- Departments
- Units
- Centers of Excellence
- Emergency – Outpatient
- Nursing Service
- Ambulances
- Patients
- Hygeia
- Υπηρεσίες
- Ιατρικά Τμήματα & Υπηρεσίες
Arteriovenous Malformations
Arteriovenous malformations are collections of abnormally weak blood vessels that form high flow shunts between arteries and veins. These bleed easily, presenting with haematomas and sometimes epilepsy. An untreated lesion is almost certain to cause death or brain damage at some time during a patients lifetime. Surgical removal is sometimes possible if the lesion is small and superficial but risks are very high for deeper lesions. These can be occluded by embolisation if the feeding vessels are few and accessible to catheters. However embolisation is frequently incomplete or closure of some vessels causes others to open up.
Gamma Knife is appropriate for well-defined arteriovenous malformations less than 3cm diameter. It offers an effective and safer method of treatment. The only significant risk (2-4%) is one of transient inflammation around the target, occurring 6-12 months after treatment.
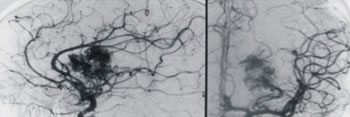
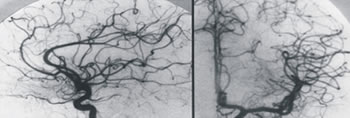
Arteriogramm demonstrating a thalamic AVM before (left) and after (right) Gamma Knife treatment
There has been a very long experience of Gamma Knife treatment of AVM because accurate stereotactic localization was possible from angiography before the advent of CT and MRI. The first lesion was treated in 1972. This large experience has made it possible to develop computer programs to predict the results of treatment (1) and in particular the probability of total occlusion, the risk of radiation damage and the risk of haemorrhage before occlusion occurs. It is therefore possible for all units to calculate the dose that has the greatest chance of success and the lowest rate of complications.
Favourable factors for success of radiosurgery are lower flow, compact or plexiform lesions, multiple shunts or fistulas and few draining veins. Gamma Knife is particularly indicated when lesions are inaccessible to surgery and embolisation, or when a residual nidus remains after other treatment. It is also important to stress that the risk of radiosurgery is less than other methods and so it is appropriate as a primary treatment unless contraindicated, for example a single high flow fistula is best managed endovascularly.
Many groups have published similar results (1-3). Total obliteration in lesions less than 3cm diameter should be 40% at one year, 80% at 2 years and 90% at 3 years. Smaller lesions have a higher success rate and lower complication rate. The risk of local oedema due to radionecrosis is 2-4% and the risk of rebleeding within 2 years is also 2-4%. Associated epilepsy is usually abolished. Success and risk are strongly related to total dose and lesion size, rebleeding is inversely related to dose. For this reason smaller lesions, which can safely tolerate a higher dose, are more effectively treated.
The indications for microsurgery are certainly very limited now; mainly compact lesions at or near the convexity of the brain in non-eloquent areas. However it is not possible to say any one treatment is dominant. It is often necessary, especially in large lesions, to rely on multimodality treatment (4). In particular, embolisation followed after 3 months by Gamma Knife (to allow time for collaterals to open) has been a productive combination. It is evident that, for the best results, a team experienced in microsurgery, embolisation and Gamma Knife surgery should evaluate patients.
REFERENCES
- Karlsson B. Gamma knife surgery of cerebral arteriovenous malformations. Thesis, Karolinska Institute, Stockholm 1996.
- Pollock BE. Patient outcomes after arteriovenous malformation radiosurgery. In Lunsford LD, Kondziolka D, Flickinger JC (eds) Gamma knife brain surgery. Prog Neurol Surg, Basel, Karger 1998; 14: 51-59.
- Chang JH, Chang JW, Park YG et al. Factors related to complete occlusion of arteriovenous malformations after gamma knife surgery. J Neurosurg 2000; 93 (suppl 3): 96-101.
- Chang SD, Marcellus ML, Marks MP et al. Multimodality treatment of giant intracranial arteriovenous malformations. Neurosurgery 2003; 53: 1-13.
- Kondziolka D, Lunsford LD, Flickinger JC et al. Reduction of haemorrhage risk after stereotactic radiosurgery for cavernous malformations. J Neurosurg 1995; 83: 825-831.
- Kida Y, Kobayashi T, Tanaka T. Radiosurgery of symptomatic angiographically occult vascular malformations with gamma knife. In Kondziolka D (ed), Radiosurgery, Basel, Karger 1995; 1:207-217.
- St George EJ, Perks J, Plowman PN. Stereotactic radiosurgery XIV: the role of the haemosiderin ‘ring’ in the development of adverse reactions following radiosurgery for intracranial cavernous malformations: a sustainable hypothesis. Br J Neurosurg 2002; 16: 385-391.
- © 2007-2024 HYGEIA S.M.S.A.
- Personal Data Protection Policy
- COOKIES Policy
- Terms of Use
- Privacy Policy
- Credits
- Sitemap
- Made by minoanDesign
Ο ιστότοπoς μας χρησιμοποιεί cookies για να καταστήσει την περιήγηση όσο το δυνατόν πιο λειτουργική και για να συγκεντρώνει στατιστικά στοιχεία σχετικά με τη χρήση της. Αν θέλετε να λάβετε περισσότερες πληροφορίες πατήστε Περισσότερα ή για να αρνηθείτε να παράσχετε τη συγκατάθεσή σας για τα cookies, πατήστε Άρνηση. Συνεχίζοντας την περιήγηση σε αυτόν τον ιστότοπο, αποδέχεστε τα cookies μας.
Αποδοχή όλων Άρνηση όλων ΡυθμίσειςCookies ManagerΡυθμίσεις Cookies
Ο ιστότοπoς μας χρησιμοποιεί cookies για να καταστήσει την περιήγηση όσο το δυνατόν πιο λειτουργική και για να συγκεντρώνει στατιστικά στοιχεία σχετικά με τη χρήση της. Αν θέλετε να λάβετε περισσότερες πληροφορίες πατήστε Περισσότερα ή για να αρνηθείτε να παράσχετε τη συγκατάθεσή σας για τα cookies, πατήστε Άρνηση. Συνεχίζοντας την περιήγηση σε αυτόν τον ιστότοπο, αποδέχεστε τα cookies μας.




































