- HYGEIA
- Vision & Mission
- Timeline
- Organizational structure
- Press Releases
- Social responsibility
- Awards and Distinctions
- Human Resources
- Scientific & Training activities
- Articles – Publications
- Our Facilities
- Magazines
- Healthcare Programs
- Doctors
- Services
- Medical Divisions & Services
- Imaging Divisions
- Departments
- Units
- Centers of Excellence
- Emergency – Outpatient
- Nursing Service
- Ambulances
- Patients
Rheumatoid arthritis
What is rheumatoid arthritis?
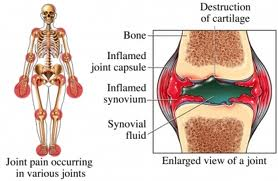
Rheumatoid arthritis is an autoimmune disease that causes inflammation in your joints. Its main symptoms are joint pain and swelling, as well as stiffness in the mornings. Τo understand how rheumatoid arthritis develops, it helps to understand how a normal joint works first.How does a normal joint work?
A joint is where 2 or more bones meet. Your joints let your bones move freely but within limits.
The ends of your bones are covered with cartilage, which has a very smooth, slippery surface. The cartilage allows the ends of your bones to move against each other almost without friction. The joint is surrounded by the synovium, which produces a small amount of synovial fluid that nourishes the cartilage and lubricates the joint. The synovium has a tough outer layer called the capsule that, together with the ligaments, holds your joint in place and stops the bones moving too much.
What happens in a joint affected by rheumatoid arthritis?
Rheumatoid arthritis causes inflammation in the synovium. The result is very similar to inflammation that you may have seen if you’ve had an infected cut or wound – it goes red, swell, produce extra fluid and hurt.
The redness is caused by the flow of blood increasing. As a result, the inflamed joint may feel warmer than usual. The inflammation is caused by a build-up of fluid and cells in the synovium, causing swelling and difficulty in moving. Your joint hurts for 2 reasons:
• Your nerve endings are irritated by the chemicals produced by the inflammation.
• The capsule is stretched by the swelling in your joint.
When the inflammation goes down, the capsule stays stretched and can’t hold your joint in its proper position. This can make your joint unstable, and it can move into unusual or deformed positions. What are the symptoms of rheumatoid arthritis?
What are the symptoms of rheumatoid arthritis?
Common symptoms of rheumatoid arthritis include:
• painful, swollen joints (small joints if the upper and lower limbs; large joints, such as knees, elbows and shoulders; and spine)
• stiffness
• tiredness (fatigue), depression and irritability
• anemia
• flu-like symptoms, such as feeling generally ill, feeling hot and sweating.
Less common symptoms include:
• weight loss
• eye inflammation
• rheumatoid nodules
• inflammation of other parts of your body
Symptoms of rheumatoid arthritis tend to come and go. You may have flare-ups when your symptoms become worse than normal and then subside.Rheumatoid arthritis varies from one person to another but it usually starts quite slowly. A few joints – often your fingers, wrists or the balls of your feet – become uncomfortable and may swell, often intermittently, while there is usually symmetry in affected joints. You may also feel stiff when you wake up in the morning.
For about 1 in 5 of those with rheumatoid arthritis the condition develops very rapidly, with pain and swelling in a lot of joints, severe morning stiffness and great difficulty doing everyday tasks.
If you have painful, swollen joints and stiffness in the morning that lasts for longer than half an hour, you should see your rheumatologist. Research shows that the sooner you start treatment for rheumatoid arthritis, the more effective it’s likely to be, so early diagnosis is important.
Since rheumatoid arthritis may affect other parts of the body apart from joints, you must tell your doctor all the symptoms your are experiencing, even if you do not believe they may relate to the condition.
Who gets it?
Rheumatoid arthritis can affect adults at any age, but most commonly starts between the ages of 40 and 50. About three times as many women as men are affected.
Genetic factors alone do not cause rheumatoid arthritis, even if it is related to some genes. This means that if a parent has rheumatoid arthritis, it does not necessarily mean that their children will be affected. The genes we inherit from our parents alone do not cause rheumatoid arthritis, but may increase the likelihood of developing the condition.
Even if you have an identical twin, who shares all the same genetic material as you, and they have rheumatoid arthritis, you only have a 1 in 5 chance of developing it too. And if some of your family have it, the severity can be very different from person to person.There’s some evidence that lifestyle factors may affect your risk of developing the condition. Rheumatoid arthritis is more common in people who:
• smoke
• eat a lot of red meat
• drink a lot of coffee
Rheumatoid arthritis is less common in people who:
• have a high vitamin C intake
• drink alcohol in moderationWhat causes rheumatoid arthritis?
Rheumatoid arthritis is an autoimmune disease, which means the body’s immune system, under certain conditions and factors (viruses, bacteria, stress) which have not been fully clarified, starts attacking the body’s own tissues, causing inflammation.
Inflammation normally dies down fairly quickly but in rheumatoid arthritis it becomes a long-term (chronic) process. The genes you inherit from your parents don’t cause rheumatoid arthritis but they may increase your chances of developing it.What is the outlook?
Studies on a large patient sample have shown that:
• 75% of people will continue having some joint pain, swelling and flare-ups.
• 20% will always have very mild rheumatoid arthritis.
• 5% will develop severe disease with extensive disability.Because rheumatoid arthritis can affect different people in different ways, we can’t predict its development, progress and prognosis.
Blood tests and X-rays will help your doctor assess how fast your arthritis is developing and what the potential outlook for your future is. This will also help your doctor to decide which form of treatment to recommend.
Most people can have periods of months or even years between flare-ups, when there’s little inflammation, although damage can still be caused in these periods. However, most people, especially if they receive appropriate treatment, will have relatively few symptoms and will be able to lead full lives.
People with rheumatoid arthritis have a slightly greater chance of having a heart attack or stroke. The risk is probably reduced by controlling the disease, for example with drug treatments. High cholesterol and smoking increase the risk, so it’s a very good idea to eat a balanced diet and stop smoking.How is rheumatoid arthritis diagnosed?
No single test can give a definite diagnosis of rheumatoid arthritis in the early stages of the condition. Doctors have to arrive at a diagnosis based on your symptoms, a physical examination and the results of X-rays and blood tests.
Blood tests
Blood tests can:
• assess the inflammation erythrocyte sedimentation rate (ESR, CRP)
• assess the gravity of the condition/prognosis (Ra test and anti CCP)
• indirectly assess the complications of the inflammation (e.g. anemia)
• assess the effectiveness of treatment and any possible side-effects
About 8 out of 10 people with rheumatoid arthritis have a positive Ra test, but about 1 in 20 people without rheumatoid arthritis also have positive results. Only about half of all people with rheumatoid arthritis have a positive rheumatoid factor when the disease starts. In addition, with regard to the CCP antibodies, they may be present for years before the condition develops and imply more severe development.X-rays and other tests
X-rays will show any damage caused to your joints by the inflammation in rheumatoid arthritis. It is necessary to have X-rays performed on all affected joints as soon as the condition appears. The changes often show up in X-rays of your feet before they appear in other joints, so your doctor may want to X-ray your feet even if they’re not causing you any problems. X-ray damages. Any damage is evident from the onset of the condition, that is why X-rays are necessary.
Doctors also evaluate imaging techniques, such as magnetic resonance imaging (MRI) scans and ultrasound scans, to see how useful they are for early diagnosis and monitoring the condition’s progress. They may be more widely used in the future.
You may need repeat blood tests and X-rays from time to time to help your doctor assess how quickly your arthritis is developing and whether you need any changes to your medication.
What treatments are there for rheumatoid arthritis?
Although there’s no cure for rheumatoid arthritis yet, a variety of treatments are available that can slow down the condition and keep joint damage to a minimum. The earlier you start treatment, the more effective it’s likely to be.Drugs
Four main groups of drugs are used to treat rheumatoid arthritis:
• painkillers (analgesics)
• non-steroidal anti-inflammatory drugs (NSAIDs)
• disease-modifying anti-rheumatic drugs (DMARDs)
• steroids
Most people with rheumatoid arthritis need to take more than 1 drug. This is because different drugs work in different ways. If you take 2 or more anti-rheumatic drugs they can be more effective than just taking 1 and there are no extra side-effects.
Your drug treatment may be altered from time to time depending on how active your arthritis is or in response to changes in your circumstances. For example, you may be advised to stop taking a particular drug if you need surgery or have a feverish inflammation.Painkillers
Painkillers alone aren’t enough to treat rheumatoid arthritis, but they’re useful for topping up the pain-relieving effects of other, more specific drugs. Paracetamol is most often used. You may take it by itself, alongside other tablets or as a compound analgesic in which it’s added to codeine or other drugs.
Non-steroidal anti-inflammatory drugs (NSAIDs)
NSAIDs reduce pain and swelling, and they start working within a few hours. The effect of some will only last a few hours but others are effective all day. Your doctor will help you to find the preparation and dose that are right for you.
NSAIDs are usually taken as tablets or capsules and you should take them with a glass of water, with or shortly after food. You can also get NSAID creams and gels that can be applied directly to the painful area. Rarely are they prescribed as an injection.
Like all drugs, NSAIDs can sometimes have side-effects. Your doctor may prescribe another medication alongside the NSAID, which will help to protect your stomach.Disease-modifying anti-rheumatic drugs (DMARDs)
DMARDs act by treating the underlying disease rather than treating your symptoms. They’re not painkillers, but they’ll reduce pain, swelling and stiffness over a period of weeks or months by slowing down the disease and its effects on your joints. They do not have an immediate effect.
There are two types of DMARDs:
• conventional DMARDs
• biological therapies
Conventional DMARDs include:
• hydroxychloroquine
• methotrexate
• sulfasalazineBecause these drugs are slow-acting, it’s important to keep taking them even if they don’t seem to be having an effect.
Some conventional DMARDs are called immunosuppressant drugs because they dampen down your immune system. They may cause side-effects, so you’ll need careful monitoring when you’re taking them. Examples of immunosuppressantDMARDs include:
• azathioprine
• leflunomide
• cyclosporineBiological therapies target individual molecules involved in the processes of inflammation and joint damage. Some biological therapies are called anti-TNF drugs, and these target a protein called tumor necrosis factor, which increases inflammation when excess amounts are present in your blood or joints. Anti-TNF drugs include:
• adalimumab
• certolizumab pegol
• etanercept
• golimumab
• infliximabOther biological therapies target different proteins:
• abatacept
• rituximab
• tocilizumabYou’ll only be given biological therapies if you haven’t responded to conventional DMARDs or you’ve had side-effects from them. They’re often given in combination with a conventional DMARD, such as methotrexate.
The side-effects of DMARDs include:
• nausea or stomach upsets
• high blood pressure
• skin rashes
• headaches
• dizzinessWhen taking any of the biological therapies, you may also experience some of the following:
• sore throat
• fever
• wheeziness
• unexplained bruises, bleeding or paleness
• symptoms of infection
• local irritation at the injection siteA number of DMARDs affect the immune system so you’ll be more likely to pick up infections. DMARDs can sometimes affect the blood or the liver, and because of this you’ll need regular medical supervision when you’re taking them. This may include regular blood and/or urine tests, so as to rule out any risks to your health from possible side-effects. However, with careful supervision, these drugs are well-tolerated and very effective.
Steroids (cortisone)
Steroids have a very powerful effect in reducing inflammation and although they don’t cure the condition they will suppress it. They can be given as injections into a joint, a vein or a muscle, or as tablets.
Cortisone injections have few side-effects but they may include:
• thinning and other changes in the skin at the site of the injection (atrophy)
• facial flushing
• interference with the menstrual cycle
• changes in moodThe side-effects of cortisone tablets can also include:
• weight gain
• osteoporosis
• muscle weakness
• cataracts
• a rise in blood sugar or blood pressure
• increased vulnerability to infectionsDoses of cortisone tablets are kept as low as possible to keep the risk of side-effects to a minimum. Your doctor may also advise that you take calcium and vitamin D supplements or anti-osteoporosis drugs to help protect your bones against osteoporosis.
You shouldn’t stop taking your cortisone tablets or alter the dose unless your doctor recommends it. It can be dangerous to stop steroids suddenly.
Physical therapies
Looking after your joints is very important in the treatment of rheumatoid arthritis. Exercise is an important part of this, and a physiotherapist can suggest different exercises that may help ease your symptoms and improve the flexibility of your joints.
A podiatrist can help with problems with your feet and ankles. They can suggest appropriate footwear for both daily life and sport.
If you’re having difficulty with day-to-day activities an occupational therapist can suggest ways that you could do them without putting too much strain on your joints. They can also give you information on splints if you need supports for your hands and wrists.
Surgery
Surgery is occasionally needed for rheumatoid arthritis. Operations vary from quite minor ones such as the release of a nerve or a tendon to major surgery such as joint replacement.
Self-help and daily living
Patients must:
• strike a balance between rest and exercise
• eat a balanced diet and keep to a healthy weight
• protect their joints from unnecessary strain
• get a good night’s sleep to help with fatigue
• learn about their conditionYour symptoms may tend to come and go with no particular pattern. Sometimes your flare-ups will have an obvious cause, such as another illness or stress, but usually there’s no obvious trigger. This unpredictability makes it difficult to plan ahead.
It’s tempting to do all your jobs when you’re having a good day, but overdoing things on the good days can be counter-productive, causing a flare-up of symptoms the next day. Pacing yourself is important. Make it clear to your family and friends that not all days are the same. It’s important they realize that activities you enjoy on a good day may be impossible on a bad one.
The effects of any condition can be mental as well as physical, and people with rheumatoid arthritis are more likely to experience depression. How you feel mentally can also affect how you feel physically, so if you feel down or depressed, it can make your symptoms harder to cope with. Don’t be embarrassed to talk about this with your doctor if you’re feeling low – managing how you feel is as important as managing the physical symptoms.
There are support groups available if you want to meet other people who have rheumatoid arthritis, and you might find that information on pain management helps you to stay positive.
Managing a flare-up
Over time you may get better at noticing the early signs of a flare-up. Sometimes a few days rest are all you need, though it’s important to do gentle exercise to help relieve stiffness. Don’t forget that you can take painkillers, and applying hot or cold pads to affected joints may ease pain too. Make sure you don’t apply them directly to the skin to avoid injury.
If you’re having regular flare-ups, you should mention this to your doctor. It may be that you need to review your treatment.
Exercise
Strike a balance between rest and exercise. Rest will make inflamed joints feel more comfortable, but without movement your joints will stiffen and your muscles will become weaker. You need to find out what the right balance is for you.
Exercise is good for your general health, so use your muscles and joints as much as you can without harming them. If a particular activity causes your joints to become warm and swollen or if it causes severe pain, then stop and rest. If not, you should be fine to continue. If a particular activity always causes a flare-up, then it’s probably best to avoid it and find an alternative.If you go to a gym or health club, tell the fitness instructor about your condition so that they can develop an appropriate exercise plan for you. Your physiotherapist can advise you about this too. It’s best to avoid exercises involving hard impacts, such as step exercises. The following activities will have less strain on your joints:
• swimming
• aquarobics (aerobics in a swimming pool)
Whichever form of exercise you do, make sure you always warm up properly.Diet and nutrition
No specific diet will cure rheumatoid arthritis, although there’s some scientific evidence that certain diets may help the symptoms in some people. The diets most likely to help have:
• low saturated fats
• high unsaturated fats, especially fish body oils (suggested intake is 1.5 g per week)
• a good supply of vitamin C
There’s some evidence that a very strict vegetarian diet can help, and people who eat a lot of red meat may have a slightly increased risk of rheumatoid arthritis. Speak to your doctor or a dietitian before starting any strict diet as the disadvantages may outweigh the advantages.
Occasionally some people find that a specific type of food upsets them, but this is quite unusual. If you think you may have an intolerance to a particular food try removing it from your diet for about 3-4 weeks and then reintroducing it. If you do have an intolerance you will notice a flare-up in your arthritis within a few days.
We recommend keeping to a healthy weight because it’ll help reduce the strain on your joints.Complementary medicine
Many people with rheumatoid arthritis try different types of complementary medicine. Most types haven’t proven effective, but there are a couple that have some scientific evidence to support their use, including:
• fish body oil
• evening primrose oil
• acupuncture
• massage
Homeopathy hasn’t been proven to relieve the symptoms of rheumatoid arthritis.Supports, aids and gadgets
It’s very important to protect your joints from unnecessary strain. An occupational therapist can give you advice about changing the way you do some tasks and on using simple aids or adaptations to make them easier.
A huge variety of gadgets are available to help with daily tasks, whether you’re at work, around the home or in the garden.Sleep
You may experience severe tiredness (fatigue) and suffer disturbed sleep. Lack of restful sleep can make it all the more difficult to cope with the pain of arthritis. Try the following tips:
• Painkillers or a warm bath can help ease pain or stiffness before going to bed.
• Check that your bed is supportive and comfortable, and if your neck and shoulders are stiff or painful, try experimenting with different pillows.
• Try to establish a relaxing bedtime routine – avoid eating, drinking tea, coffee or alcohol and smoking close to bedtime.
• Regular exercise should help you to sleep, but don’t exercise within 3 hours of going to bed.
You can discuss your sleep problems with your doctor. Although doctors are reluctant to prescribe sleeping tablets for long-term use, they can be useful for short spells when a lack of sleep is a serious problem.If you’re stiff when you wake up, try these exercises while lying in bed:
1. Bend 1 leg at the knee. Hold your other leg straight and lift your foot just off the bed. Hold for a slow count of 5 then lower. Repeat 5 times with each leg.
2. Lie on your back. Pull each knee to your chest in turn, keeping your other leg straight.
3. If you’re able to, lie on your back, hands behind your head (or by your side if your shoulders are painful). Bend your knees and, keeping your feet on the floor, roll your knees slowly to one side. Hold this position for 10 seconds. Repeat this 3 times for each side.Sex and pregnancy
There’s no reason why you should stop having sex. You may find that some positions are more comfortable than others, so experiment to find out what works for you. Tiredness may affect your desire for sex, so talk to your partner. Good communication is the key to resolving any difficulties.
The contraceptive pill won’t make a difference to your arthritis or its treatment so it’s fine to keep taking it. If you do decide you want a baby, discuss your plans with your doctor before you want to start a family as some drugs can temporarily reduce fertility. Other drugs, such as methotrexate and leflunomide, can affect the baby’s development so it’s important to use reliable contraception if you take these.
Most mothers with rheumatoid arthritis feel better during pregnancy, though symptoms are likely to return once the baby is born. Any flare-up of symptoms after the birth can usually be dealt with quickly.
Work
It’s usually possible to keep on working, unless it involves a lot of manual labor.
- © 2007-2024 HYGEIA S.M.S.A.
- Personal Data Protection Policy
- COOKIES Policy
- Terms of Use
- Privacy Policy
- Credits
- Sitemap
- Made by minoanDesign
Ο ιστότοπoς μας χρησιμοποιεί cookies για να καταστήσει την περιήγηση όσο το δυνατόν πιο λειτουργική και για να συγκεντρώνει στατιστικά στοιχεία σχετικά με τη χρήση της. Αν θέλετε να λάβετε περισσότερες πληροφορίες πατήστε Περισσότερα ή για να αρνηθείτε να παράσχετε τη συγκατάθεσή σας για τα cookies, πατήστε Άρνηση. Συνεχίζοντας την περιήγηση σε αυτόν τον ιστότοπο, αποδέχεστε τα cookies μας.
Αποδοχή όλων Άρνηση όλων ΡυθμίσειςCookies ManagerΡυθμίσεις Cookies
Ο ιστότοπoς μας χρησιμοποιεί cookies για να καταστήσει την περιήγηση όσο το δυνατόν πιο λειτουργική και για να συγκεντρώνει στατιστικά στοιχεία σχετικά με τη χρήση της. Αν θέλετε να λάβετε περισσότερες πληροφορίες πατήστε Περισσότερα ή για να αρνηθείτε να παράσχετε τη συγκατάθεσή σας για τα cookies, πατήστε Άρνηση. Συνεχίζοντας την περιήγηση σε αυτόν τον ιστότοπο, αποδέχεστε τα cookies μας.




































