- HYGEIA
- Vision & Mission
- Timeline
- Organizational structure
- Press Releases
- Social responsibility
- Awards and Distinctions
- Human Resources
- Scientific & Training activities
- Articles – Publications
- Our Facilities
- Magazines
- Healthcare Programs
- Doctors
- Services
- Medical Divisions & Services
- Imaging Divisions
- Departments
- Units
- Centers of Excellence
- Emergency – Outpatient
- Nursing Service
- Ambulances
- Patients
- Hygeia
- Υπηρεσίες
- Ιατρικά Τμήματα & Υπηρεσίες
Systemic lupus erythematosus (SLE)
There are two main forms of lupus:
• discoid lupus, which only affects your skin
• systemic lupus erythematosus (SLE), which affects your skin and joints and often also involves your internal organs including your heart or kidney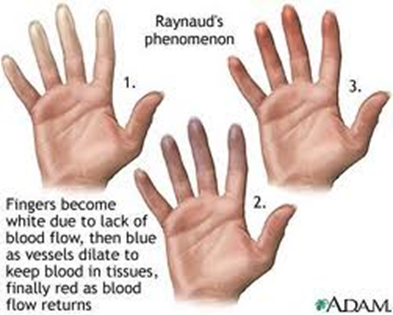 This section only deals with the systemic type of lupus.
This section only deals with the systemic type of lupus.Lupus occurs when your immune system attacks your body’s own tissues. It can cause inflammation in many different parts of your body, though most people will only have a few of the possible symptoms.
Systemic lupus erythematosus (SLE), often known just as lupus, is an autoimmune disease where your immune system produces antibodies that attack your body’s own tissues, causing inflammation.
Lupus usually affects your skin and joints, but it may also involve your heart or kidneys, when the effects can be severe. SLE isn’t the same as discoid lupus, which only affects the skin.What are the symptoms of lupus?
Symptoms can include
• joint pain
• a skin rash
• extreme tiredness (fatigue)
• fever
• weight loss
• headaches
• mouth ulcers
• hair loss
• swelling of lymph glands
• your fingers or toes changing color in cold conditions (Raynaud’s phenomenon)
Lupus can affect many different parts of your body. If your heart, brain or kidneys are affected, it can be much more serious, but most people will only have one or a few of the following symptoms. Many people will find that the symptoms come and go.Skin and mouth
• a rash over parts of your body that are exposed to the sun – a butterfly-shaped rash over your cheeks and the bridge of your nose is especially common
• your fingers changing color in cold weather, going first very pale, then blue and finally red – this is called Raynaud’s phenomenon
• groups of mouth ulcers, which may come back repeatedly
• Sjögren’s syndrome – this affects around 1 in 8 people with lupus and causes a dry mouth and eyes
Hair
Some hair loss is common and can be severe, but once a flare-up is under control your hair will usually grow back.Joints
Joint pain is common, especially in the small joints of your hands and feet. The pain tends to move from joint to joint and is often described as flitting. Lupus doesn’t usually cause joints to become permanently damaged or deformed. About 1 in 20 people with lupus develop more severe joint problems. Fewer than 1 in 20 have hypermobile joints or a form of arthritis called Jaccoud’s arthropathy, which can change the shape of your joints.Kidneys
Around 1 in 3 people with lupus have significant inflammation of their kidneys, and kidney damage can sometimes occur. Most people with inflammation can be successfully treated if it’s spotted early through regular tests.Blood and blood vessels
• high blood pressure, particularly if your kidneys are involved
• a raise in your cholesterol level – you should have this checked yearly
• anemia and a reduction in the number of platelets and/or white blood cells – these tend to be more common in children
• blood clots in your veins or arteries, usually caused by antiphospholipid antibodies – some of these autoantibodies can also affect pregnancy, causing an increased risk of miscarriage (antiphospholipid syndrome)
• Cortisone tablets, which are often used to treat lupus, can also cause an increase in blood pressure.Brain and nervous system
• migraines (affects 1 in 3)
• anxiety or depression
• dizziness
• memory loss or confusion
• fits (similar to epilepsy) or feelings of paranoia (similar to schizophrenia) – these only affect a small number of peopleHeart and lungs
• inflammation in the lining tissues around your heart (pericarditis) and lungs (pleurisy), both of which cause breathlessness and sharp chest pains
• large amounts of fluid developing in these lining layers, causing severe breathlessness, but this is rare
• narrowing of your blood vessels, leading to an increased risk of angina, heart attacks and strokesOther organs
• swelling of your lymph glands
• abdominal pain, caused by effects on your gut, pancreas, liver or spleen
• a painful red eye or changes in your eyesight
• an autoimmune disease that affects your thyroid gland, in particular the type which makes the gland underactive (affects fewer than 1 in 10)
• rheumatoid arthritis or inflammation of your muscles (myositis) – this is rareHow is lupus diagnosed?
Lupus can mimic other, more common conditions, so you’ll probably have a number of tests before the diagnosis is confirmed.
No specific test can diagnose lupus. Your doctor will make the diagnosis based on the history of your illness, a physical examination and blood tests. Test results help to distinguish lupus from other conditions that may have similar symptoms.
A number of different blood tests may be used:
• Anti-nuclear antibody (ANA) test
About 95% of people with lupus are ANA positive, but the test can sometimes be positive in people without lupus so it can’t confirm the diagnosis.
• Anti-double-stranded DNA (anti-dsDNA) antibody test
About 75% of people with lupus have these antibodies. A positive test means that it’s highly likely that you have lupus. The level usually goes up when lupus is more active, so repeat tests may be helpful in monitoring your condition and deciding on treatment.
• Anti-Ro antibody test
If you test positive for this autoantibody, you may be more likely to get skin rashes and to suffer from Sjögren’s syndrome. It can pass across the placenta in pregnancy. If you carry it and decide to have a baby, your pregnancy will be more closely monitored.
• Antiphospholipid antibody test
A positive test for these autoantibodies may mean an increased risk of miscarriage and developing blood clots.
• Complement level test
Complement refers to a set of proteins in the blood that protect us from infections. Levels go down when lupus is more active.
• Erythrocyte sedimentation rate (ESR) test
This measures inflammation. The ESR is often raised in lupus.
• Kidney and liver function tests
These include blood and urine tests. They’re carried out regularly so that any problems caused by your condition or the drugs you’re using can be recognized and dealt with quickly.
• Blood cell counts
Hemoglobin, white and red blood cells and platelets are all made in the bone marrow, so blood cell counts can help to show whether the bone marrow is affected by your condition or the drugs you’re using to treat it.
These tests can also be helpful in monitoring your condition after diagnosis.
A variety of tests are available to check the function of your heart, lungs, liver and spleen. Depending on which organs your doctor thinks may be involved, you may have X-rays, an ultrasound scan, a computerized tomography (CT) scan or a magnetic resonance imaging (MRI) scan.
A urine test can show if there’s protein or blood in your urine. This can help doctors to recognize a problem in your kidneys at a very early stage. You may need further tests, such as kidney filtration tests.If you have the following symptoms, your doctor may take a biopsy of lymph gland tissue to rule out cancer:
• fever
• weight loss
• swelling of the lymph glandsWhat treatments are there for lupus?
Treatment is with a combination of drugs and self-help measures, which will vary depending on your particular symptoms.Drugs may include:
• anti-inflammatory drugs
• cortisone tablets, creams or injections
• drugs which suppress your immune system
• drugs to control high blood pressure and high cholesterol
There’s no cure for lupus at present, but the condition is very treatable. It usually responds well to a number of different types of drugs, especially when treatment is started early.Drugs
The drugs you use will depend on how severe your condition is and which parts of your body are affected. Your treatment will probably be changed or adjusted as your symptoms flare-up up or improve.
Non-steroidal anti-inflammatory drugs (e.g. naproxen, ibuprofen)
• reduce inflammation
• help with symptoms in your joints
• often used for short periods
Steroid creams (cortisone)
• useful for skin rashes
Antimalarials (e.g. hydroxychloroquine)
• reduce inflammation
• used alone or with cortisone creams for skin rashes
• also useful as a treatment for fatigue and joint pain
• can help protect your heart
Steroid tablets (e.g. cortisone)
• used for short periods for complications such as pleurisy or pericarditis
• may also be used as a longer term treatment for other problems, such as kidney inflammation or severe blood problems.
Immunosuppressive drugs (e.g. azathioprine, cyclosporine, cyclophosphamide, methotrexate, mycophenolate)
• used to suppress your immune system
• may need to be taken for long periods, though the dose may be reduced if your condition becomes less active
• will often control high blood pressure and help prevent kidney problems
• may be used along with steroid tablets to allow steroid dose to be reduced
Biological therapies (e.g. rituximab)
• removes B-cells (a type of white blood cell that produces harmful autoantibodies)
• widely used when conventional immunosuppressive drugs aren’t effectiveCortisone injections
• can be injected into a muscle or vein as immediate treatment to help control a flare-up
• can also be injected into your scalp if hair loss is a problem
Anti-hypertensive drugs
• may be used to control high blood pressure
Treatments for Raynaud’s phenomenon (e.g. nifedipine tablets, iloprost injections)
• may be used to widen your blood vessels to improve circulationWhat about side-effects?
All drugs have some potential side-effects, and you and your doctor will need to balance the risk of side-effects with the need to control the condition. Sometimes this may mean taking additional medications to protect against the side-effects of others.
If you’re taking NSAIDs your doctor may prescribe a drug called a proton pump inhibitor (PPI), which will help to protect your stomach.
If you’re taking cortisone tablets, you may be given bisphosphonates, calcium tablets and vitamin D tablets to guard against osteoporosis.Having lupus will make you more prone to infection, especially if you’re taking immunosuppressive drugs. Take sensible precautions and avoid contact with family and friends when they have infectious diseases like chickenpox.
You shouldn’t have live vaccines if you’re on more than 10 mg of prednisolone daily or immunosuppressive drugs. These vaccines include yellow fever, live typhoid and live oral poliomyelitis (polio). You should think about this when you’re planning a holiday. Check with your doctor if you think you might need these vaccinations.
Pneumovax (which gives protection against the most common cause of pneumonia) and yearly flu vaccines are well tolerated and recommended.Other treatments
If joint pain is a particular problem, acupuncture may help. Your pain relief may only last a short time to begin with but repeated treatments may bring longer term benefit.
If there’s a large build-up of fluid in the lining tissues of your heart or lungs, this may need to be drained using a needle and syringe.Very rarely, some people with lupus can develop kidney failure, which may require dialysis or a kidney transplant. Severe kidney damage can usually be prevented by early diagnosis and treatment.
Self-help and daily living
You can help yourself by:
• not smoking
• protecting your skin from strong sunlight with white clothes, a hat, sunglasses and high SPF sunscreen
• dressing to keep your hands and feet warm in cold weather
• resting when the condition is most active but otherwise taking regular exercise
• pacing yourself and planning your activitiesManaging a flare-up
Lupus naturally improves and worsens at different times. Learning how to manage a flare-up is important to help you be more in control of your condition. The reasons for a flare-up can vary, but the following can play a part:
• exposure to sunlight
• too little rest
• infections
• stress
Try to identify the things that lead to a flare-up and find ways of managing or avoiding them.Fatigue
If your fatigue has a specific cause, such as anemia or an underactive thyroid gland, this can be identified by a blood test and treated. If no specific cause can be identified, fatigue may be more difficult to deal with. Some medications, like hydroxychloroquine, and learning to pace yourself can help.
Exercise improves fitness and stamina and can help in overcoming fatigue, but you’ll need to start very gently – ask to see a physiotherapist for advice about suitable exercises.Smoking
Many of the problems caused by lupus can be made worse by smoking:
• Lupus and smoking can both cause your blood vessels to narrow, causing circulatory problems and increasing your risk of strokes and heart attacks.
• Lupus can make you more vulnerable to respiratory infections, while smoking leads to long-term lung damage, which can make these infections more frequent and more severe.
• If lupus affects your kidneys, it can lead to high blood pressure. Smoking can also contribute to high blood pressure, increasing the risk of strokes and worsening kidney disease.
Giving up smoking is one of the most important things you can do to reduce the risk of the more serious complications. It can be extremely difficult to stop, but treatments are available that can help you. Talk to your GP or call a smoking helpline for advice.Exercise
When lupus is active, you may not feel like doing very much and it’s important to rest when you need to. But too much rest will cause the muscles to weaken and may make you feel more tired. You need to find the right balance between rest and exercise. Walking and swimming are good exercises because they can improve fatigue, fitness and stamina without putting too much strain on the joints. Even when you’re having a flare-up, a small amount of exercise is helpful. You should have some gentle exercise that you can do even on a bad day.Diet and nutrition
There’s some evidence that a diet low in saturated fat and supplemented by fish body oil may be helpful.
Be careful of any exclusion diets where you stop eating large food groups. Lupus is an active autoimmune disease and you need all the nutrients that a well-balanced diet will provide. Consult a dietitian if you need more specific advice.Sunlight
Too much ultraviolet light can cause a rash and flare-ups of symptoms in the internal organs. Bear this in mind when you choose a holiday destination and talk to your rheumatology nurse specialist or dermatologist if you’re in doubt. When you’re outside, use the following tips:
• Keep out of the midday sun and wear a hat.
• Cover your skin or use a sun-blocking cream, SPF 50 or greater. You can also buy tinted high-factor sun creams that can be used as foundation make-up.
• Avoid sitting under sun umbrellas on a paved area because the sunlight will be reflected onto your face.
Raynaud’s phenomenon
If you experience symptoms of Raynaud’s phenomenon in your hands or feet, make sure you dress suitably for cold weather. Smoking is bad for your circulation and is likely to make your symptoms worse. Regular exercise will improve your circulation.Stress
Even if it doesn’t affect the course of your condition, emotional stress can make it seem worse. Learn how to manage any stress in your life. Your doctor may be able to refer you to a psychologist who can help with coping strategies.Meeting others with lupus
Lupus is a difficult condition to live with and throws up many challenges, especially during periods of life when you may need more energy. Meeting others with lupus doesn’t necessarily remove these challenges but it can help you to cope with them by sharing your thoughts and concerns with someone who understands. You may meet people through an education program or patient support groups.Contraception
If you have lupus you should use contraceptive pills that contain only progesterone or low-dose estrogen, or consider physical/barrier methods of contraception. This is because estrogen can increase the chances of a flare-up.
Hormone replacement therapy (HRT)
It’s safe to use HRT for short periods if symptoms of the menopause are severe and your lupus is otherwise well controlled.- © 2007-2024 HYGEIA S.M.S.A.
- Personal Data Protection Policy
- COOKIES Policy
- Terms of Use
- Privacy Policy
- Credits
- Sitemap
- Made by minoanDesign
Ο ιστότοπoς μας χρησιμοποιεί cookies για να καταστήσει την περιήγηση όσο το δυνατόν πιο λειτουργική και για να συγκεντρώνει στατιστικά στοιχεία σχετικά με τη χρήση της. Αν θέλετε να λάβετε περισσότερες πληροφορίες πατήστε Περισσότερα ή για να αρνηθείτε να παράσχετε τη συγκατάθεσή σας για τα cookies, πατήστε Άρνηση. Συνεχίζοντας την περιήγηση σε αυτόν τον ιστότοπο, αποδέχεστε τα cookies μας.
Αποδοχή όλων Άρνηση όλων ΡυθμίσειςCookies ManagerΡυθμίσεις Cookies
Ο ιστότοπoς μας χρησιμοποιεί cookies για να καταστήσει την περιήγηση όσο το δυνατόν πιο λειτουργική και για να συγκεντρώνει στατιστικά στοιχεία σχετικά με τη χρήση της. Αν θέλετε να λάβετε περισσότερες πληροφορίες πατήστε Περισσότερα ή για να αρνηθείτε να παράσχετε τη συγκατάθεσή σας για τα cookies, πατήστε Άρνηση. Συνεχίζοντας την περιήγηση σε αυτόν τον ιστότοπο, αποδέχεστε τα cookies μας.